Lower Abdominal Pain and Fatigue in IBS
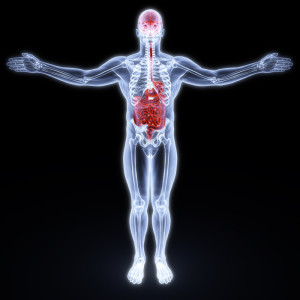
Could lower abdominal pain and fatigue be linked?

© Can Stock Photo
One of the most common places for IBS sufferers to get pain is in the lower abdomen (i.e. your lower belly). What a lot of people don’t realize is that the fatigue and weakness they feel could be connected to that pain.
We’re going to discuss that, but first a warning:
If you haven’t seen a doctor about your abdominal pain you should be doing that, not reading this! It can be serious!
There. Now that’s out of the way. If you’re still here, then…
You need to know about the vagus nerve.
The vagus nerve has nothing to do with Las Vegas :), it’s a nerve that runs from your lower abdomen up to your brain.
And it’s connected to your bowels.
Pain in the lower abdomen can cause you to feel week and woozy (okay dizzy then ;). This is called a vasovagal episode,
© Can Stock Photo
a vasovagal response, or a vasovagal attack.
The symptoms of such an attack are:
- Sweating
- Nausea
- Weakness or fatigue
- Dizziness
- Light headedness
- Other less common symptoms
Why you feel so tired when you have bowel pain:
What happens is that the pain in your lower belly convinces your brain that you’re injured or ill in your belly. The brain then sends more blood to that area (bloating anyone?), which can leave less blood for other important tasks.
Like not fainting.
That’s right, the pain in your abdomen can make you feel weak, nauseous and tired. I remember attacks where I could barely function! It was all I could do to keep my head off the table.
Did he say fainting???

© Can Stock Photo
Yes.
You know that abdominal pain that is so severe? It can actually cause you to pass out!
Lower abdominal pain can cause a vasovegal attack, but a severe attack can lead to fainting. That’s called vasovegal syncope.
The pain gets bad enough that your brain and your vagus nerve decide to spend all your physical resources on whatever is causing it. The next thing you know, you wake up feeling disoriented, embarrassed, and hopefully uninjured!
Why isn’t fatigue commonly listed as an IBS symptom?
Frankly, I don’t know the answer to that puzzle.
I know two people personally, that faint completely away and wake up on the floor from pain associated with diarrhea or constipation. I know several others that have lower abdominal pain and fatigue.
The doctor’s never seem to mention it when discussing IBS though. Sorry, I just don’t know why.
What you can do about lower abdominal pain and fatigue:
Well, the first thing you can do is avoid foods or drinks that upset your bowels. But once you have the pain, what can you do?
I can’t prescribe treatment, but I can tell you what helps me. I use a heating pad and and some anti-inflammatory, like ibuprofen and it works wonders.
They don’t always completely remove the pain and fatigue of an IBS attack, but they help with the pain!
Some people swear by peppermint oil which clinical studies show can soothe the bowels.
There are also some anti-spasmodic drugs that help ease cramps. You will have to talk to your doctor about those though, because they are prescription only.
IBS pain can cause fatigue, or at least it does in my world.
I hope this helps you solve your fatigue puzzle.
Read more about IBS symptoms.
Find out about foods that can trigger IBS.
16 Replies to “Lower Abdominal Pain and Fatigue in IBS”
Were any of you tested for H Pylori?
Thank you soooooooooo much for this simple, straightforward, and empathetic description of a problem that has been plaguing me now ever since I developed what I’m guessing is rampant IBS about a year and a half ago. Like another of your commenters stated, I too used to be fairly healthy and strong, but most days now it’s all I can do to keep myself from going back to bed after breakfast ?. I developed an infected wound after knee replacement surgery, and as a result was put on IV vancomycin for one week. My poor gut has never been the same. I went from a hearty vegetarian who could eat bushels of grains and veggies to a quivering mouse afraid to eat a sliver of anything green lest I explode. And the fatigue!!! I could never explain why I would need to go immediately to my bed the minute the abdominal pain would come on?!?!?! And of course, my doc thinks it’s all in my head (when she even has time to listen to me, that is ?). Thank you, thank you, thank you. At least I now know the connection , and no longer feel like I’m crazy ☺️!
Thanks a lot Shawn for explaining in detail about all the symptoms. I have been fainting with all the other symptoms since a few years and no one had any explanation for it. Finally I have an answer and closure. Thanks and God Bless you!
Thank you for this Article as it describes what happens to me during a Flare Up, total weakness, shaking, fatigue and difficulty standing up.
It’s been over a year since Mr. Francis wrote his comment, but I have to remark that it seems doctors will assign anything they don’t want to deal with to the “in the patient’s head” file.
Thank you very, very much for your article, Mr. Author. It answered the question I’ve been asking in vain for years.
I have had all the symptoms minus fainting since my early forties after a bacterial infection of the prostate (prostatitis) and the intestine . The IBS started Immediately and has bothered me for 20 years ……….. until recently: I started to notice that I would feel better after using antibiotics , and specifically after a series of tooth abscess where the dentist prescribed Spiramycine/metronidazole. It took a couple of years and abscess to make the connection, but after a treatment the IBS symptoms would be reduced dramatically for 3 months. My doctor was VERY skeptical but thought it might be the Metronidazole that was working , which is sometimes used for travelers diarrhea. We tried that with no luck: It was the Spiramycine & Metronidazole that was working. After making a fuss I got a renewable prescription and started taking a course of pills about every 4 months when the IBS would reoccur in force , I am now down to about twice a year and I feel not perfect but MUCH BETTER! , My doctor thinks it is in my head….its not!
Good luck,
John
John; I noticed the exact same thing except I have used tetracycline at times for rosacea and I felt much better after a short course. I have used flagyl a few times as an experiment previously and had mixed results, but mostly good. I like the vagal nerve theory but I am suspicious there is some sort of infective component also that triggers the episode, otherwise why would antibiotics work? I would love to have a study done of people that experience the extreme fatigue and abdominal pain and see if there is a common pathogen in the gi tract that might be responsible.
Thanks,
Dean
I visited doctors for many years, but none of them could explain my reaction to lower abdominal pain: feeling weak in the calves of my legs, and then standing up and sitting down on the toilet rapidly for as long as the abdominal pain lasted. Your explanation of blood flowing to the bowels is probably what’s happening, and has given me some closure.
I’m very glad you found the information helpful. Sometimes not knowing is the worst part.
a tea spoon of ginger root juice work very well when i have ibs pain to cure it you need to avoid the food that cause it for me it’s dairy and tomatos and flour as well..
to cure it i eat artichoke heart 3 time a week for 1 month and the inflamation going away
stomach pain will make you very weak
good luck!
That sounds like an excellent tip, Gilles. Thank you!
This is exactly what I’m going through. I used to be strong as an ox…now I’m weak as a lamb…cant wait to get in bed and relax. I heard about the peppermint oil…I’m going to try it.
Yes. It’s VERY frustrating. I hope the peppermint oil helps. Let us know back here if it does if you remember. Thanks!
You’re right that the average doctor does not discuss fatigue or, for that matter, any other non-GI symptom of IBS, but reputable academic researchers of IBS certainly do know that many non-GI symptoms of various sorts do occur in people with IBS at statistically higher rates than people with IBS and chronic fatigue syndrome/chronic fatigue immune dysfunction syndrome/myalgic encephalomyelitis (whichever one’s preferred term for the same disorder) is one of many commonly overlapping conditions. But one does not have to have a comorbid diagnosis to be unduly tired most of the time as a secondary effect of IBS. And this is a problem, because the typical interventions suggested for IBS pain and bowel disturbances may or may not help a person with fatigue or other non-GI symptoms.
If you or anyone wishes to check out my blog, I have a category for non-GI and overlapping conditions. There is also an article from the University of North Carolina Center for Functional GI and Motility Disorders linked on the main IBS Impact site, IBS page. Please feel free to browse other posts and pages also.
Thanks Nina, for that well informed and useful bit of info.
I know that I’LL be checking out your blog shortly.
Regards,
Shawn
I’ll check out your blog. Looks like a good resource!